What Is Malaria?
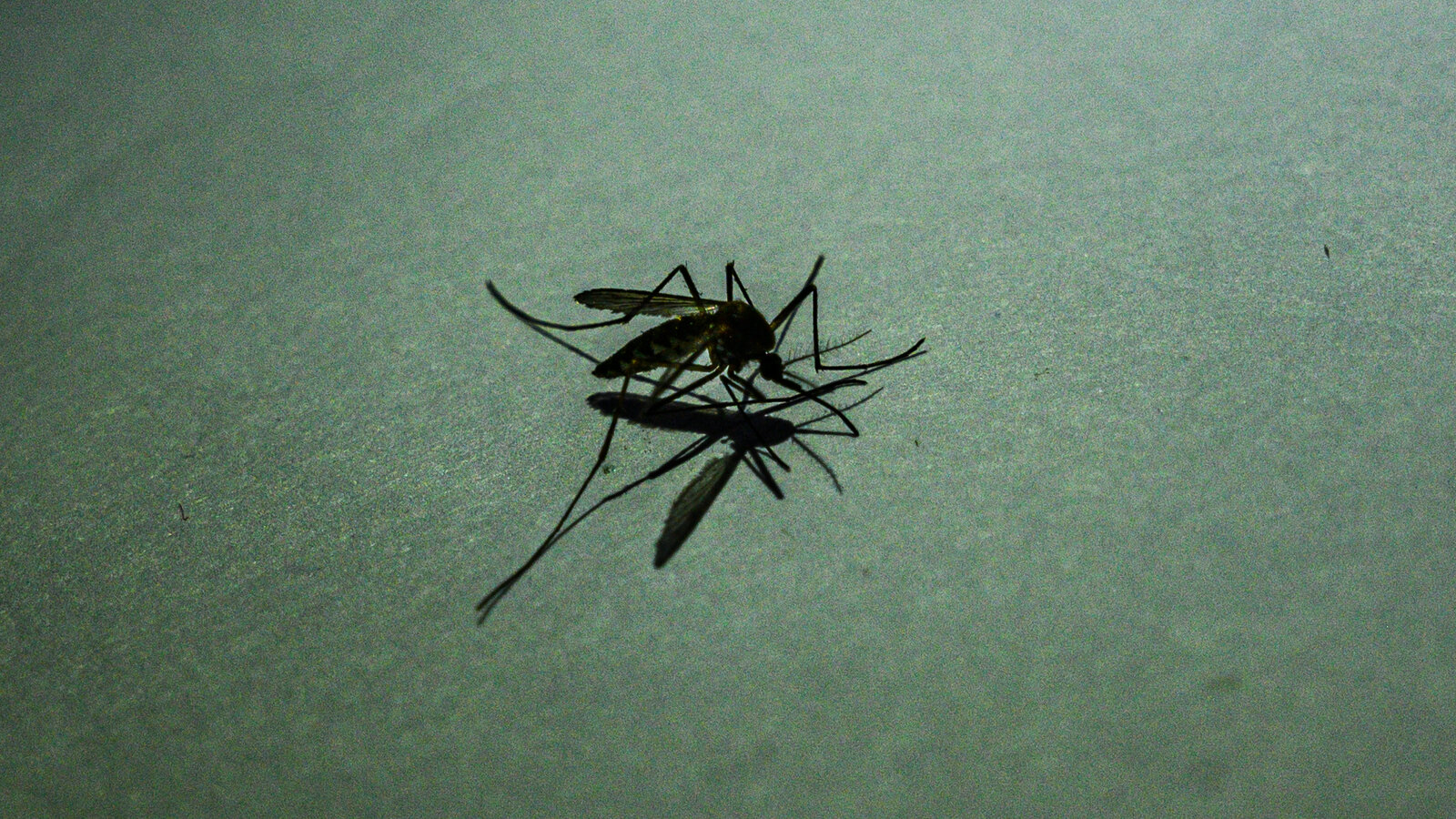
Malaria is a serious disease spread by bites from infected mosquitoes. Although it’s rare in the U.S., travelers to certain parts of the world, like Africa (south of the Sahara Desert), South America, and Southeast Asia, are at risk. Malaria thrives in warm climates where the parasite-carrying Anopheles mosquitoes live.
Every year, about 2,000–2,500 people in the U.S. are diagnosed with malaria, mainly returning travelers. Globally, malaria causes about 608,000 deaths annually, mostly in regions without easy access to treatment.
In rare cases, malaria can spread in the U.S. through local mosquitoes that pick up the parasite from an infected traveler. For example, in 2023, nine cases were reported in Florida, Texas, and Maryland.
How to Prevent Malaria
Preventive medications, like pills taken before, during, and after your trip, can help protect you. Additional prevention tips include:
- Wear protective clothing: Cover as much skin as possible.
- Use insect repellents: Effective options include DEET, picaridin, or oil of lemon eucalyptus. Avoid using these on young children under three years old.
- Sleep under bed nets: Choose nets treated with insecticides for extra protection.
- Take malaria pills: Your doctor can recommend the right medication based on your destination.
What Causes Malaria?
Malaria is caused by Plasmodium parasites, spread through bites from infected female Anopheles mosquitoes. There are five main species that infect humans:
- P. falciparum: The most severe type, causing life-threatening complications like cerebral malaria (brain damage). Common in Africa.
- P. vivax: Can lie dormant in the liver and cause relapses months or years later. Found in Asia, Latin America, and parts of Africa.
- P. ovale: Similar to P. vivax but can’t infect people with the Duffy blood group. Found in West Africa and the Pacific.
- P. malariae: Causes chronic infections that can last a lifetime. Found worldwide.
- P. knowlesi: Found in Southeast Asia, it primarily infects monkeys but can cause severe illness in humans.
How Malaria Spreads
Most infections occur when bitten by an infected mosquito. Rarely, it can also spread through:
- Blood transfusions or organ transplants
- Sharing contaminated needles
- From a pregnant person to their baby during delivery
Malaria is not contagious like the flu or a cold. You can’t catch it through casual contact or sex.
Malaria Life Cycle
Malaria follows a cycle:
- A mosquito bites an infected person, picking up the parasite.
- About a week later, the mosquito bites another person, passing on the parasite.
- Once in the body, parasites travel to the liver, multiply, and enter red blood cells.
- The infected red blood cells burst, releasing more parasites, causing symptoms.
Who Is at Risk?
About half of the world’s population (3.3 billion people) is at risk of malaria, especially in warm regions like:
- Sub-Saharan Africa
- South and Southeast Asia
- Central and South America
- Parts of the Middle East and Oceania
Certain groups face a higher risk of severe malaria, including:
- Babies and young children
- Pregnant people
- Those with weakened immune systems (e.g., HIV/AIDS patients)
- Travelers from regions without malaria
People in high-malaria regions can develop partial immunity, but this fades if they move away.
Symptoms of Malaria
Symptoms typically appear 10–15 days after a bite but can be delayed for months in some cases (P. vivax). Common symptoms include:
- Fever and chills
- Sweating
- Nausea, vomiting, or diarrhea
- Fatigue
- Headaches and body aches
- Jaundice (yellow skin)
- Seizures or confusion (in severe cases)
When to See a Doctor
If you suspect malaria, especially after traveling to a high-risk area, see a doctor immediately. Severe symptoms like impaired consciousness, dark urine, or difficulty breathing need urgent medical attention.
Diagnosing Malaria
Doctors diagnose malaria through:
- Blood smears: The most accurate method, where a lab checks your blood for parasites.
- Rapid diagnostic tests (RDTs): Quick finger-prick tests, but they might need confirmation with a blood smear.
- Molecular tests (PCR): These detect parasite DNA and confirm the species.
- Antibody tests: Show past malaria infections.
- Drug resistance tests: Check which medicines will work on the parasite.
Malaria Treatment
Treatment depends on:
- The parasite species
- The severity of your symptoms
- Your location and medical history
Common medications include:
- Chloroquine or hydroxychloroquine: For sensitive strains.
- Artemether-lumefantrine (Coartem) or atovaquone-proguanil (Malarone): For resistant strains.
- Primaquine: Targets parasites in the liver to prevent relapses.
- Artesunate: An IV treatment for severe cases.
Severe infections may also require hospitalization and additional treatments like IV fluids.
Complications of Malaria
Serious complications include:
- Cerebral malaria (brain swelling and damage)
- Organ failure (liver, kidney, spleen)
- Severe anemia
- Low blood sugar
Malaria Prevention Tips
To lower your risk:
- Use preventive medicines: Follow your doctor’s recommendations.
- Protect yourself from bites: Use insect repellents, nets, and long clothing.
- Avoid high-risk travel if pregnant: Malaria increases the risk of complications like miscarriage.
Malaria Vaccines
The World Health Organization (WHO) recommends two malaria vaccines—RTS,S/AS01 and R21/Matrix-M—for children in areas with high P. falciparum rates. Vaccines have significantly reduced child deaths in Africa, but insecticides and bed nets remain crucial.